The Connection Between Chronic Pain and PTSD
The Albany Clinic • July 1, 2022
If you have post-traumatic stress disorder (PTSD), you may know that you’re at an increased risk for a variety of other disorders, including depression and anxiety . But did you know that there is also a correlation between PTSD and some physical conditions, such as IBS and chronic pain ?
While the reasons behind the link between chronic pain and PTSD aren’t entirely known, it has been proven that they are related. In fact, a study in the Psychiatric Times has shown that the prevalence of chronic pain among patients with PTSD may be as high as 80% .
This can be due to a variety of factors, including the way that chronic pain affects the brain. Unfortunately, many people do not realize they have both conditions or how the two conditions affect each other. Keep reading to learn about the relationship between chronic pain and PTSD.
What Is PTSD?
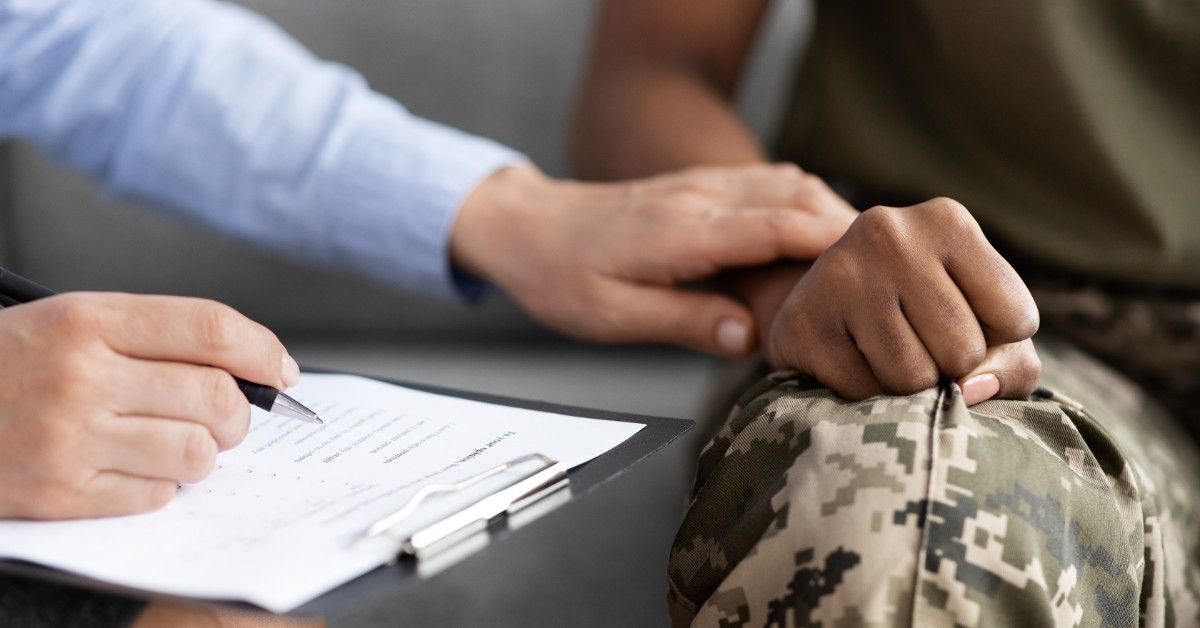
PTSD is a mental health condition that’s triggered by a traumatic event. This could be a single life-changing event, such as a car crash, robbery, or near-death experience, or it can manifest from a series of traumas, such as childhood abuse or military service. Both experiencing or witnessing an event can cause PTSD.
Symptoms of PTSD include flashbacks, nightmares, and severe anxiety, as well as uncontrollable thoughts about the event. It can lead to problems with memory and concentration, making it hard to continue with everyday activities. It can also cause insomnia, irritability, and avoidance of anything that reminds you of the trauma.
What Is Chronic Pain?
Chronic pain is defined as any pain that lasts for more than six months. It can be caused by an injury, a health condition, or even psychological factors. In most cases, it constantly persists for weeks, months, or years, which causes a significantly lower quality of life for the sufferer. Common types of chronic pain include:
- Arthritis
- Back pain
- Nerve pain
- Headaches and migraines
- Stomach pain
Chronic pain can be extremely debilitating, making it hard to concentrate, sleep, or even perform basic tasks. The pain can vary in intensity and may come and go over time. Chronic pain may, over time, lead to psychological effects, including depression, anxiety, anger, and fear of making an injury worse.
The Link Between PTSD and Chronic Pain
There are a few theories on how PTSD and chronic pain may be linked . The following are a few of the most popular ones.
Pain Caused by a Traumatic Event
The most obvious explanation for the link between chronic pain and PTSD is when the pain is sourced from the traumatic event that caused the PTSD. This event could be a car accident, a fall, or any other type of physical trauma. The pain may be caused by an injury sustained during the event or could develop over time.
Shared Vulnerabilities
Studies show that PTSD and chronic pain could have shared underlying vulnerabilities. Anxiety sensitivity, or the tendency to respond to an event with fear, may amplify the emotional response someone has to a traumatic event, which increases the risk of both conditions developing.
Feelings of loss of control and a lowered physiological threshold for alarm due to trauma can also cause hypervigilance and muscle tension, increasing the chances of chronic pain developing.
Pain Sensitivity Differences
Research shows that patients with PTSD often experience hyperarousal (a prolonged state of the flight-or-fight response staying triggered) and dissociation, both of which can increase or decrease pain perception. For patients with reduced pain perception, chronic pain can more easily develop and impact quality of life more severely.
Mutual Maintenance and Exacerbation
Finally, PTSD and chronic pain may be linked simply because the two conditions happen to have symptoms that may exacerbate each other.
Pain may serve as a traumatic trigger, especially for patients whose trauma stemmed from a physically painful event, which can cause hyperarousal and fear. This hyperarousal and fear may, in turn, cause a patient to focus on their pain more than usual. Hyperarousal by itself can also cause prolonged muscle tension, leading to the development of chronic pain.
Treatment Options
PTSD can have a profound effect on your mental health, but it can also lead to physical symptoms such as gastrointestinal problems, headaches, chest pain, and other types of chronic pain.
While the specific reasons behind these symptoms vary, the chronic stress PTSD generally puts your body through leads to an increased likelihood of developing chronic pain.
When dealing with both PTSD and chronic pain, treatment methods can be a bit difficult to navigate. Few options tackle both issues at once, and sometimes treatment for one can get in the way of treatment for another. Nevertheless, the following are a few methods that have proven successful.
Therapy
Cognitive-behavioral therapy , or CBT, is a type of therapy that has been shown to be effective in treating both PTSD and chronic pain. This form of therapy focuses on helping you change the negative thoughts and beliefs you have about your condition.
CBT can help you develop new coping mechanisms for dealing with your chronic pain, as well as provide you with tools to deal with your PTSD symptoms.
Lifestyle Changes
Making lifestyle changes is another crucial step in managing both PTSD and chronic pain. Exercise, relaxation techniques, and a healthy diet can all help improve your symptoms.
Exercise can be especially helpful in treating chronic pain, as it releases endorphins, which are natural painkillers. Relaxation techniques, such as yoga and meditation, can also help you manage your pain by helping you focus on something other than your symptoms.
Medications
There are a few different types of medications that can be used to treat both PTSD and chronic pain.
Anti-inflammatory drugs, such as ibuprofen, can help reduce inflammation, which can in turn help relieve pain. Antidepressants and anti-anxiety medications can also be useful in treating both conditions.
Other options, such as opioid painkillers and sedatives, may be necessary for patients with more severe symptoms. However, these medications come with a high risk of abuse and addiction, so they should only be used as a last resort.
The post The Connection Between Chronic Pain and PTSD appeared first on The Albany Clinic.